This genetic stuff is confusing, I know! A lot of people do not understand it, they assume EB is an autoimmune condition or Nicky gets rashes etc, so I want to attempt at writing my own version of explaining EB in laymen’s terms. I am a fan of those Dummies books!
So, here goes:
What is EB?
EB stands for Epidermolysis Bullosa (ep-ih-dur-MOL-uh-sis buhl-LOE-sah). Mouthful, no? Most people cannot pronounce it, so most parents and Doctors just use the acronym “EB”.
The name is derived from the latin words epidermis (the outer layer of our skin), lysis (loosening or breakdown) and bullosa (blister). Hence, Epidermolysis Bullosa means the breakdown and blistering of the epidermis.
This is all fine and dandy, but it’s not entirely accurate. There are three major forms of EB: Simplex, Junctional & Dystrophic, and the only form that blisters in the epidermis is the Simplex form. Junctional’s blisters are in between the epidermis and the dermis, and Dystrophic’s blisters form in the dermis, which is the layer below the epidermis.

EB Skin Structure
It’s also very important to note that EB is just an ‘umbrella’ word. A word that throws together all blistering conditions no matter how they are inherited or how they manifest themselves. Back in the late 1800s and early 1900s, when the words “Epidermolysis Bullosa” first appeared, the Doctors told patients they had EB if they blistered. It’s like if Doctors bunched up together all conditions which feature rashes (eczema, psoriasis, rosacea or shingles) or conditions that feature the progressive deterioration of nerve cells (Tay-Sacks Disease, Parkinson’s & ALS).
Because of this it’s extremely important to know that each form of EB is different in the way it’s inherited, in the way it manifests itself, in the way blisters appear, in the way the wounds are to be treated, the way skin heals, in quality of life, life expectancy and so on and so forth. EB is not EB in the sense that each form, in my humble view, should be called something completely different as to discourage comparisons. After all, you cannot compare Tay-Sacks Disease with Parkinson’s, or Eczema with Shingles.
What are the types of EB?
There are three main types of EB:
Epidermolysis bullosa simplex (EBS). Caused by a defective Keratin Protein, blistering occurs in the epidermis. This is the most common type of EB, and tends to be milder than the other types. Babies can be born with mild to severe life threatening blistering but almost always improve with age. Blisters heal without scars and do not cause deformities, however they are more easily obtained. Wounds tend to heal better if not bandaged since they are more superficial. There are many types of EB Simplex and most are caused by a dominant gene mutation. So far 12 subtypes have been identified, which can all look different.
Junctional epidermolysis bullosa (JEB): Caused by a defect in the Collagen XVII, Integrin, or Laminin, blistering occurs at the junction between the epidermis and the dermis. There are many types of Junctional EB, so far 6 subtypes have been identified. Blisters can heal with scars, but do not cause deformities. Some forms of Junctional EB improve as the patient gets older, while a rare form of Junctional (Herlitz) EB can be fatal in infancy.
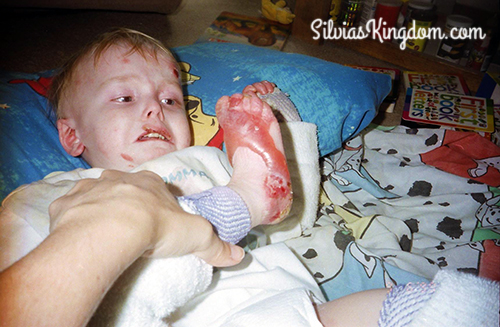
Dystrophic epidermolysis bullosa (DEB): Caused by a mutation in the Collagen VII gene, blistering occurs in the dermis. The condition can be dominant (DDEB) or recessive (RDEB), so far 12 subtypes have been identified. Both dominant and recessive forms of Dystrophic EB cause scarring. Dominant forms rarely causes deformity of the hands or feet caused by the fusion of the fingers or toes. The recessive form of Dystrophic EB is the most severe, chronic type of EB. Patients get worse and worse as they age, not because the condition worsens per se, but because the wounded areas get weaker and eventually refuse to heal in areas that receive the most trauma. Blistering begins at birth or shortly afterwards. Much of the skin is covered in blisters and there is extensive internal blistering. Children can develop deformities caused by the recurrent scarring of the fingers and toes and the hands and arms become fixed in stiff positions. Bandaging is often essential to allow proper healing of wounds. It is painfully difficult for a child with recessive Dystrophic EB to ingest food due to the internal blistering that occurs in the mouth, esophagus, and gastrointestinal tract.
How is EB inherited?
Inheritance of EB is gender and ethnic-group non-specific. There are three major ways a child can be born with EB:
1. Recessively: Recessive forms of EB include all forms of Junctional and Recessive Dystrophic. Both parents have to be carriers (have the recessive gene) and they have a 25% chance each pregnancy of passing both of their faulty EB gene to their baby.
What is a Recessive gene? A Recessive gene is a gene that lays dormant in our system until it has no choice but to ‘wake up’. We all inherit a gene for everything from each parent, and the recessive gene is one that is automatically recessive. In my case, for example, I inherited a “good” skin gene from my dad (it’s plain as day I am daddy’s girl) so this means I inherited my ‘EB skin gene’ from my mom. When the two skin genes were coupled at my conception and one had to become dominant, the EB skin gene took a bow. Hey, it likes to sleep and we want him to sleep, don’t we? They automatically sleep. In my son’s case, he unfortunately inherited my EB skin gene, and by some twist of fate, his dad also had a recessive EB skin gene, so when the two got together… one of them had no choice but waking up. This is why Recessive conditions are so rare.
2. Dominantly: Dominant forms of EB include all forms of Simplex and Dominant Dystrophic. One parent has the condition and it has a 50/50 chance to pass it on to their child. Dominant genes don’t automatically sleep or nothing. They are out and about. This is why they are more common.
3. Spontaneous Mutation: EB also can be acquired through a spontaneous mutation. That is, a child is born with a dominant genetic mutation that causes EB (it’s always a dominant mutation, never recessive), despite neither parent having EB. When this occurs, it is because the gene spontaneously mutated in either the sperm or the egg before conception. There is no scientific evidence that the parents could have prevented such spontaneous mutation, and there are no known environmental, dietary or behavioral triggers for this type of mutation. To this, I might note, years ago a Vietnam Veteran made a point to state that one of his children and a few of his friend’s children who were also Vietnam Vets were born with Simplex EB, so he wanted to find out if there could ‘possibly’ be a correlation with Agent Orange or anything they might have been exposed while at war, but no real ’cause’ was ever found.
In an effort to be complete in my descriptions, I must note there is also an extremely rare form of Dystrophic EB called ‘Aquisita’ which is not inherited but associated with autoimmunity to type VII collagen and onset occurs only in adulthood.
Remember, EB is not contagious!!
How rare is EB?
An estimated 50 in 1 million live births are diagnosed with EB. Of these cases, approximately 92% are epidermolysis bullosa simplex (EBS), 5% are dystrophic epidermolysis bullosa (DEB), 1% are junctional epidermolysis bullosa (JEB), and 2% are unclassified. For the Recessive forms, carrier frequency ranges from 1 in 333 for JEB, to 1 in 345 for RDEB (More here on carriers #s).
I hope I made this as clear as possible, if not or if you have anymore questions, please ask me! Leave a comment below. I can also answer more specific questions regarding my son who has RDEB. While I have extensively researched all forms of EB I can only truly consider myself an expert on my son.
Love & Light,